Selective serotonin reuptake inhibitor
This page has not been fully approved by the PsychonautWiki administrators. It may contain incorrect information, particularly with respect to dosage, duration, subjective effects, toxicity and other risks. It may also not meet PW style and grammar standards. |
Selective serotonin reuptake inhibitors (commonly abbreviated as SSRIs) are a class of pharmaceutical antidepressant medications. They are commonly prescribed for the treatment of major depressive disorders. Other conditions include anxiety disorders, obsessive-compulsive disorder, migraine, attention-deficit hyperactivity disorder (ADHD), addiction/dependence, and sleep disorders. The exact pharmacological mechanism of action SSRIs is unknown.[1] They are believed to increase the extracellular level of the neurotransmitter serotonin, eventually leading to improved mood.[citation needed][clarification needed]
SSRIs can be dangerous when used in combination with other substances that increase or modulate serotonin such as MDMA and Monoamine Oxidase Inhibitors (MAOIs). If SSRIs are used with these substances, it could potentially lead to serotonin syndrome, which can potentially lead to hospitalization and be fatal. SSRIs do not work for everyone and take 3-6 weeks to start having noticeable effects.[clarification needed]
SSRIs are reported to have fewer side effects than older antidepressants like monoamine oxidase inhibitors and tricyclic antidepressants.[citation needed] Monoamine oxidase inhibitors also interact with many other medications and foods, leading to a hypertensive crisis that can potentially be fatal. SSRIs can cause sexual dysfunction and compulsive yawning as side effects. Discontinuation of SSRIs can lead to withdrawal symptoms which include flu-like symptoms, as well as brain zaps.
Mechanism of action
SSRIs primarily work by inhibiting the serotonin transporter protein which leads to an increased level of serotonin, leading to downregulation of the receptor. SSRIs also lead to an increased level of cAMP (cyclic adenosine monophosphate), brain-derived neurotrophic factor, and several other regulatory neuromodulators. Different SSRIs have different binding profiles, which may lead to different effects.[2] Unlike the older tricyclic antidepressants, SSRIs are not powerful muscarinic acetylcholine receptor antagonists, so they generally have far fewer anticholinergic side effects like dry mouth (xerostomia), visual acuity suppression, and difficulty urinating.
Subjective effects
- Anxiety suppression
- Appetite enhancement or Appetite suppression
- Brain zaps - upon withdrawal.
- Cognitive fatigue
- Decreased libido
- Dream potentiation
- Ego inflation
- Mania
- Orgasm suppression - this effect is usually mild.
- Physical fatigue
- Suicidal ideation
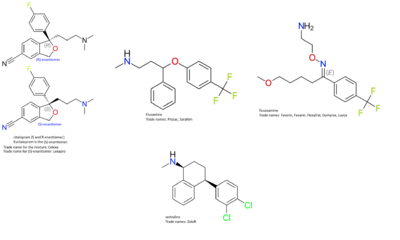
Examples
Citalopram
Citalopram is a SSRI sold under the brand name Celexa in the United States. Citalopram is indicated for the treatment of a major depressive disorder. Citalopram was approved in 1998 by the Food and Drug Administration for the treatment of major depressive disorder.[3] Citalopram is almost exclusively found as the hydrobromide salt, which is the only form approved by the FDA.[4]
Escitalopram
Escitalopram is an SSRI sold under the brand name Lexapro in the United States. Escitalopram is indicated for the treatment of major depressive disorder and anxiety disorders. It is the s-enantiomer of citalopram, and both have similar efficacy. Escitalopram was FDA approved in 2002.[5]
Fluoxetine
Fluoxetine is an SSRI commonly sold under the brand name Prozac. Fluoxetine is indicated for the treatment of major depressive disorder, bulimia nervosa, obsessive-compulsive disorder, panic disorder, and premenstrual dysphoric disorder. Fluoxetine is sometimes used in conjunction with olanzapine (an atypical antipsychotic) to treat bipolar I disorder as well as treatment-resistant depression.[6]A single pill medication called Symbyax is a combination of olanzapine and fluoxetine.[7]Fluoxetine is on the World Health Organization's list of essential medicines, a list of medicines needed for a basic and effective health system.[8]Fluoxetine was first FDA approved in 1987.
Fluvoxamine
Fluvoxamine is an SSRI that is used to treat obsessive-compulsive disorder. Fluvoxamine was first approved by the FDA in 1994.[9]Fluvoxamine has the greatest affinity for the σ1 (sigma-1) receptor, where it acts as an agonist, which may contribute to its biological effects.[10]
Paroxetine
Paroxetine is a SSRI that is sold under the brand name Paxil. Paroxetine is used to treat major depressive disorder, obsessive-compulsive disorder, post-traumatic stress disorder, anxiety disorders, premenstrual dysphoric disorder, and under the brand name Brisdelle, it is used to treat hot flashes related to menopause. Paroxetine was first approved by the FDA in 1992.[11]
Sertraline
Sertraline is a SSRI that is sold under the brand name Zoloft. Sertraline is used to treat major depressive disorder, obsessive-compulsive disorder, post-traumatic stress disorder, anxiety disorders, panic disorder, and premenstrual dysphoric disorder. Sertraline was first FDA approved in 1991.[12]Unlike most SSRIs, sertraline, has somewhat significant activity at the dopamine transporter protein[13] and could be considered a serotonin-dopamine reuptake inhibitor.
Other SSRIs
Several other SSRIs have been developed and marketed. Dapoxetine is used in some countries to treat premature ejaculation. Indalpine and zimelidine were originally marketed but later withdrawn for Guillain–Barré syndrome. Cericlamine and panuramine were developed but never marketed.
Drug interactions
A wide array of substances is contraindicated with SSRIs. substances that increase extracellular serotonin may increase the risk of serotonin syndrome, particularly substances like MDMA, dextromethorphan, tramadol and pethidine. Independent research should be done before taking any substances while on a SSRI to ensure there is no drug interaction. Some dietary supplements such as 5-HTP and St. John's Wort can lead to serotonin syndrome if taken by someone currently medicated with a SSRI.
Some NSAID analgesics may increase the risk of excess bleeding in those who take SSRIs. NSAIDs include acetaminophen (paracetamol), ibuprofen, aspirin, and naproxen.
Most SSRIs inhibit the function of certain cytochrome P450 enzymes that metabolize other substances so that SSRIs may lead to an increased or decreased serum level of certain medications.
See also
External links
References
- ↑ http://pi.lilly.com/us/prozac.pdf page 20
- ↑ Kolb, Bryan and Wishaw Ian. An Introduction to Brain and Behavior. New York: Worth Publishers 2006, Print.
- ↑ Nemeroff, CB (2012). Management of Treatment-Resistant Major Psychiatric Disorders. USA: Oxford University Press. p. 30.
- ↑ Citalopram | https://www.drugs.com/citalopram.html
- ↑ Escitalopram | https://www.drugs.com/cdi/escitalopram.html
- ↑ Fluoxetine | https://www.drugs.com/fluoxetine.html
- ↑ Symbyax Prescribing Information | http://pi.lilly.com/us/symbyax-pi.pdf
- ↑ WHO List of Essential Medicines | http://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf
- ↑ Fluvoxamine | https://www.drugs.com/cdi/fluvoxamine.html
- ↑ Sigma-1 receptors and selective serotonin reuptake inhibitors: clinical implications of their relationship. | https://www.ncbi.nlm.nih.gov/pubmed/20021354
- ↑ Paroxetine | https://www.drugs.com/paroxetine.html
- ↑ Sertraline | https://www.drugs.com/sertraline.html
- ↑ Second generation SSRI: human monoamine transporter binding profile of escitalopram and R-fluoxetine | https://www.ncbi.nlm.nih.gov/pubmed/12232544