Talk:Tilidine: Difference between revisions
>Terephtalat m added opiate Interactions |
>Terephtalat m added SUmmaryCheat |
||
| Line 1: | Line 1: | ||
{{headerpanel|{{DepressantOD|opiates}}}} | {{headerpanel|{{DepressantOD|opiates}}}} | ||
{{SummarySheet}} | |||
{{SubstanceBox | {{SubstanceBox | ||
Revision as of 22:27, 23 September 2023

Fatal overdose may occur when opiates are combined with other depressants such as benzodiazepines, barbiturates, gabapentinoids, thienodiazepines, alcohol or other GABAergic substances.[1]
It is strongly discouraged to combine these substances, particularly in common to heavy doses.
| Summary sheet: Tilidine |
| Tilidine | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |
|||||||||||||||||||||||||||||||
| Chemical Nomenclature | |||||||||||||||||||||||||||||||
| Common names | Tilidine, Tilidin, Darby, Valoron, Generika | ||||||||||||||||||||||||||||||
| Substitutive name | Tilidine | ||||||||||||||||||||||||||||||
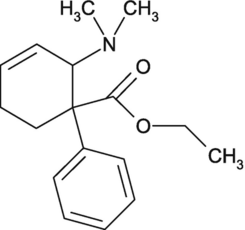
| Systematic name | (E)-2-(Dimethylamino)- 1-phenyl-cyclohex-3-en- 1-carbonsäureethylester | ||||||||||||||||||||||||||||||
| Class Membership | |||||||||||||||||||||||||||||||
| Psychoactive class | Opioid | ||||||||||||||||||||||||||||||
| Chemical class | Opioid | ||||||||||||||||||||||||||||||
| Routes of Administration | |||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
| Interactions | |||||||||||||||||||||||||||||||
Tilidine (also known as Ethyl-6-(dimethylamino)-3,6-dihydro-[1,1`-biphenyl]-1(2H)-carboxylat) is a synthetic opioid
Tilidine is an opioid pain medication used to relieve moderate to severe pain. It's often combined with naloxone to reduce the risk of misuse. As with any opioid, it should only be used under the supervision of a healthcare professional and as prescribed, as it can be habit-forming and has potential side effects.
Dangerous interactions
Warning: Many psychoactive substances that are reasonably safe to use on their own can suddenly become dangerous and even life-threatening when combined with certain other substances. The following list provides some known dangerous interactions (although it is not guaranteed to include all of them).
Always conduct independent research (e.g. Google, DuckDuckGo, PubMed) to ensure that a combination of two or more substances is safe to consume. Some of the listed interactions have been sourced from TripSit.
- Alcohol - Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Memory blackouts are likely
- Stimulants - Stimulants increase respiration rate which allows for a higher dose of opiates than would otherwise be used. If the stimulant wears off first then the opiate may overcome the user and cause respiratory arrest.
- Benzodiazepines - Central nervous system and/or respiratory-depressant effects may be additively or synergistically present. The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position blackouts/memory loss likely.
- DXM - Generally considered to be toxic. CNS depression, difficulty breathing, heart issues, and liver toxicity have been observed. Additionally if one takes DXM, their tolerance of opiates goes down slightly, thus causing additional synergistic effects.
- GHB/GBL - The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position
- Ketamine - Both substances bring a risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
- MAOIs - Coadministration of monoamine oxidase inhibitors (MAOIs) with certain opioids has been associated with rare reports of severe adverse reactions. There appear to be two types of interaction, an excitatory and a depressive one. Symptoms of the excitatory reaction may include agitation, headache, diaphoresis, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremor, diarrhea, hypertension, tachycardia, seizures, and coma. Death has occurred in some cases.
- MXE - MXE can potentiate the effects of opioids but also increases the risk of respiratory depression and organ toxicity.
- Nitrous - Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position. Memory blackouts are common.
- PCP - PCP may reduce opioid tolerance, increasing the risk of overdose.
- Tramadol - Increased risk of seizures. Tramadol itself is known to induce seizures and it may have additive effects on seizure threshold with other opioids. Central nervous system- and/or respiratory-depressant effects may be additively or synergistically present.
- Grapefruit - While grapefruit is not psychoactive, it may affect the metabolism of certain opioids. Tramadol, oxycodone, and fentanyl are all primarily metabolized by the enzyme CYP3A4, which is potently inhibited by grapefruit juice[2]. This may cause the drug to take longer to clear from the body. it may increase toxicity with repeated doses. Methadone may also be affected[2]. Codeine and hydrocodone are metabolized by CYP2D6. People who are on medicines that inhibit CYP2D6, or that lack the enzyme due to a genetic mutation will not respond to codeine as it can not be metabolized into its active product: morphine.
Legal status
- USA* Tilidine is not available as an approved drug in the U.S. </ref>
- Europe* In the EU Tilidine is prescribed for severe pain </ref>
- ↑ Risks of Combining Depressants - TripSit
- ↑ 2.0 2.1 Ershad, M., Cruz, M. D., Mostafa, A., Mckeever, R., Vearrier, D., Greenberg, M. I. (March 2020). "Opioid Toxidrome Following Grapefruit Juice Consumption in the Setting of Methadone Maintenance". Journal of Addiction Medicine. 14 (2): 172–174. doi:10.1097/ADM.0000000000000535. ISSN 1932-0620.